Search Results

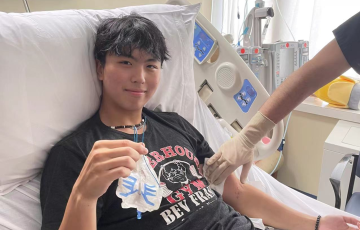
Lincoln
In the fall of 2017, Lincoln was not feeling well and had typical cold virus symptoms. He also had a recurring fever and an unexplained rash. After two trips to the pediatrician, the doctor thought he had a persistent virus and then bronchitis. On our third visit, they thought he may have mono, so bloodwork was taken, and we were told to go to Children’s Hospital immediately. We were scared and had no idea what was wrong. Cancer was not even a thought.

Annette
I had been feeling unwell for quite a while. I would come home from work and go to bed right after dinner. I would sleep for hours and still be fatigued. When we had afternoon meetings, I would fall asleep. My husband and I kept thinking it was my very stressful job. I was on airplanes three times a week and would be traveling all over the country. I wasn’t eating or sleeping well. I finally decided to take early retirement. I still did not feel well even after being retired. I finally got to the point where I was so sick, I told my husband to take me to the emergency room.
Kevin
My senior year of high school was supposed to be the best year of my life. College applications, celebrations, and memories with friends—I had it all planned out. But life had a different path in store for me. At the very start of my senior year, I was diagnosed with acute lymphoblastic leukemia (ALL), and just like that, my world changed forever.

Kim
On February 22, 2011, our 2½-year-old Abigail just stopped walking. We were baffled and took her to the pediatrician who sent us to the hospital to have her tested for a joint infection. After several hours at the ER, she was diagnosed with acute lymphoblastic leukemia (ALL). That was not what we had expected, and we worried about her identical twin as well. Eight months into Abigail’s treatment, in October of 2011, her identical twin Natasha was also diagnosed with ALL.

Paige
On September 8, 2020, my youngest baby Paige was diagnosed with high-risk B-cell acute lymphoblastic leukemia (HR B-cell ALL) at Children's National Medical Center in Washington D.C. This diagnosis came after two weeks of visually noticing a change in Paige's behavior. By that point, she had been suffering from a high fever (102-104°) for two weeks after being misdiagnosed by Patient First Urgent Care. She had extreme fatigue, complaints of sore muscles, and literally not wanting to do anything. But this discovery happened by chance.
Complications of CLL or CLL Treatment
InfectionPeople with CLL are more likely to get infections.

Lisa
It was 2009. Obama had just been sworn in as president, captain Sully successfully landed United Airlines flight 1549 on the Hudson River during an aircraft malfunction, and all souls on board survived.

Jan
After returning from a diving trip to Cyprus in November 2021, I started having headaches and sweating at night. Just two weeks later, I was diagnosed with acute leukemia and was immediately hospitalized. Two days later, I had my first round of chemotherapy as my case was pretty serious. Chemotherapy became a big part of my everyday life for the next three months.
After one week with no chemo, I started getting my life back, just partially. I made it thanks to amazing doctors, nurses, inner strength, positivity, and healthy food. Yoga breathing helped a lot too.
Molly
I did this Facebook challenge in memory of my father. He died of acute lymphoblastic leukemia (ALL) just after being diagnosed three months prior. He died on my wedding anniversary. I took care of him until the end. I am a nurse, and it made it much easier to care for him. He meant the world to me.
He loved doing anything outside. Fishing and hunting were his favorites. He was a hall-of-fame bowler, loved to golf, and enjoyed cooking on the grill. His laugh was contagious. I miss him so much every day.
Thomas
I was declared to be in remission from acute lymphoblastic leukemia (ALL) on Sept 1, 2015. To celebrate one year of remission, I biked from Waukesha, WI to Port Washington, WI, a total of 104 miles round trip.
This photo is from the deck of Smith Brothers in Port Washington, the half way point of the ride. I was joined by one of my caregivers, Maria, of St. Luke's for the first 25 miles of the ride. After the initial round of chemo in 2015, I couldn't even bike 2 miles.
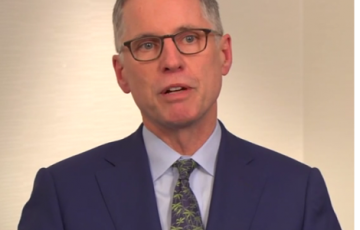
Dr. Carroll
William Carroll, M.D., is the leader of a five-year LLS Specialized Center of Research (SCOR) grant.

Janie
My name is Janie, and I was diagnosed with acute myeloid leukemia (AML) almost one year ago at 37 years old. I am married with two children and am so happy to be alive today. My story is unique, as is everyone’s; however, mine is special because my sister ended up being my 10/10 identical match, and she saved my life via transplant. I was transplanted on Aug 10, 2024, and so lucky to be home for Thanksgiving. I made it mandatory that we take family photos as family is and always has been so important to me. The photo I am sending you is of me and my sister (my donor).
Treatment Outcomes
Since the introduction of the drug Gleevec® and similar tyrosine kinase inhibitors, the number of patients with chronic myeloid leukemia (CML) who enter remission and stay in remission for years has increased dramatically over the past decade.
For survival statistics, click here.
Fertility and Pregnancy
Fertility, Pregnancy and TKIsPatients of childbearing age, as well as the parents of children with cancer, should ask their healthcare team to explain how treatment may affect fertility (the ability to have children). Patients with CML who will be taking TKIs should discuss fertility preservation with their doctors before starting TKI therapy.
Growing numbers of CML patients of childbearing age are living in stable remissions and are considering having children while being treated for CML. There is no risk that parents will pass the Ph chromosome onto their children.
Disease Complications
In medicine, a complication is a medical problem that occurs during the course of a disease or after a procedure or treatment. Possible complications of PV include:
Choosing a Blood Cancer Specialist or a Treatment Center
Taking an active role in making decisions regarding your treatment can have a positive effect on your health and quality of life. One of your first choices as an active participant in your care is to either select a specialist to manage your treatment or to choose a treatment center.
You may be seeking a blood cancer specialist or a treatment center because you:
Big Climb
No matter where you live, no matter what your connection to cancer may be, you can step up to take cancer down by being a part of The Leukemia & Lymphoma Society’s Big Climb.
Take on a new challenge, by climbing to the top of iconic buildings, all while raising critical funds towards The Leukemia & Lymphoma Society’s mission to cure leukemia, lymphoma, Hodgkin's disease, and myeloma, and improve the quality of life of patients and their families.
School
This page includes information about:

Lila
It’s January 11th, 2017, well past midnight, probably around 3 am. I am on the side of a mountain in Africa, 1000 miles away from home, in pitch black out, -20º with the winds, and I can barely feel my fingers. All I can see is the headlamp spot of light shining on the trail.
I think to myself, “Well, Lila, maybe this was not your best idea!” I look up and call my teammate in front of me, my best friend Dawn, and say, “Dawn, I am sorry I talked you into this.” She just looks at me, gives a knowing smile, then turns back to the path in front of us!

Gabriele
For approximately a year leading up to my diagnosis, I began experiencing various symptoms and was generally feeling unwell. About 3 months prior to diagnosis, my joint and bone pain started impacting my daily life heavily. I was struggling to lift my arms and walk normally. Of the many symptoms, the most extreme were breathing problems, extreme fatigue, headaches, and even passing out. I was admitted to Roswell Park Cancer Institute in April 2022 extremely neutropenic and anemic. At 26 years old I was diagnosed with acute myeloid leukemia (AML) and began chemotherapy immediately.

Wendy
I am a 3-time Hodgkin lymphoma (HL) survivor. I underwent two stem cell transplants. The first transplant was my own stem cells, the second transplant was a donor transplant. My baby sister was my donor (she was a 6/6 match); I was very lucky. I underwent three years of radiation and chemotherapy and have been in remission now 12 years. Since then, I have gotten involved with The Leukemia & Lymphoma Society (LLS). I first started by creating a fashion show to raise money for LLS.

Jeremy
Lucy was diagnosed with acute lymphoblastic leukemia (ALL) when she was 32-weeks pregnant with our son Watson. She underwent two rounds of chemo while our son was inside her. After giving birth to our healthy, 4 lb., premature baby, she immediately went back to treatment with more rounds of chemo and a bone marrow transplant. After the transplant, she had to stay in 100 days of isolation where she could only see our newborn son through a glass window and wasn’t able to touch him due to her weakened immune system.

