Inspirational Stories
Madeleine
Burkitt’s lymphoma (BL)
We were lucky. It seems strange to frame it that way, but it's true.
My 16-year-old daughter discovered a lump in her neck back in April of 2020. Because of COVID, we were reluctant to go to the doctor, and we just kept an eye on it. It didn't go away, and by late May, I called the doctor. Because many folks were avoiding doctors due to the pandemic, we were lucky, and we got in to see her pediatrician right away. She referred us to the ENT department. The ENT guy ordered an ultrasound. That wasn't conclusive, so he ordered a CT scan. That wasn't conclusive, so he ordered a needle biopsy. That wasn't conclusive, so he ordered an excisional biopsy of the lymph node (surgery!). That ended up being conclusive. All of this took less than two weeks. Lucky.
The surgery was on a Wednesday, and we were in visiting the pediatric oncologist at Doernbecher Children's Hospital in Portland, Oregon, on Friday after a second CT scan in the morning. The diagnosis was B cell lymphoma, more specifically Burkitt lymphoma (BL) which falls under the non-Hodgkin umbrella.
The second CT scan showed that the lymphoma, which is a fast-growing type, had unfortunately spread. We were admitted to Doernbecher Children's Hospital on Sunday. BL is one of the most aggressive cancers around. Luckily (there's that word again), it is also one of the most treatable cancers as well. The doctor reassured us that this cancer is highly curable and that Maddie would beat it. We are so grateful for the work of The Leukemia & Lymphoma Society (LLS) for the contributions they have made to research and caregivers. They are one primary reason this aggressive blood cancer is so highly curable among pediatric patients.
After a night of being hooked up to an IV getting hydrated, Maddie had some bone marrow aspirated and a spinal tap to see if the lymphoma cells had spread there. She also had an initial bit of chemotherapy injected right into her spinal fluid. Then, Monday night, after Maddie had a PICC line put in, she had her first full round of chemo.
The spinal tap and bone marrow showed NO lymphoma cells; this meant that her cancer was stage 3 (tumors above and below the diaphragm). A second CT scan after the first week of inpatient chemo showed a reduction in tumor size of over 60%. Tumors that previously could be felt through the skin were either barely noticeable or couldn't be felt at all! We all felt lucky! With this type of cancer, the chemo is primarily inpatient so vitals, kidney function, etc., can be watched closely.
Throughout the summer that Maddie turned 17, she spent five separate weeks in the hospital combined with several outpatient visits. She finished up her junior year of high school in the hospital, taking final exams on her laptop. She was lucky that school had gone remote so she had this option! I was lucky that my work had also gone remote, so I was with her every step of the way while continuing my job from the hospital, the oncology clinic, and our couch. We were all lucky that Doernbecher was so close to our home in Vancouver, Washington, so we could go home as needed and didn't need to get a hotel room during Maddie's hospital stays. We were lucky that her dad could continue to work and come visit every night.
As with most cancer patients, Maddie was highly susceptible to infection. We had strict instructions on what to do and who to call if Maddie spiked a fever while we were at home between treatments. Because of COVID, we were very careful. We had no visitors at the hospital or at home unless it was virtual. Everyone was already wearing masks and sanitizing their hands 80 times a day. Luckily, Maddie made it through the entire treatment without a single infection. Her doctor says she is the only patient she's ever had that made it through like that. I think it's because of COVID precautions. Lucky.
There were some hiccups along the way. Maddie had a paradoxical reaction to Versed. The drug which is supposed to ease anxiety did the exact opposite in Maddie. Luckily, her doctor agreed to full sedation for the rest of the spinal taps that Maddie required so she could get the intrathecal infusions called for. Her last inpatient stay had to be extended a few days because the methotrexate wasn't clearing her blood as quickly as it needed to.
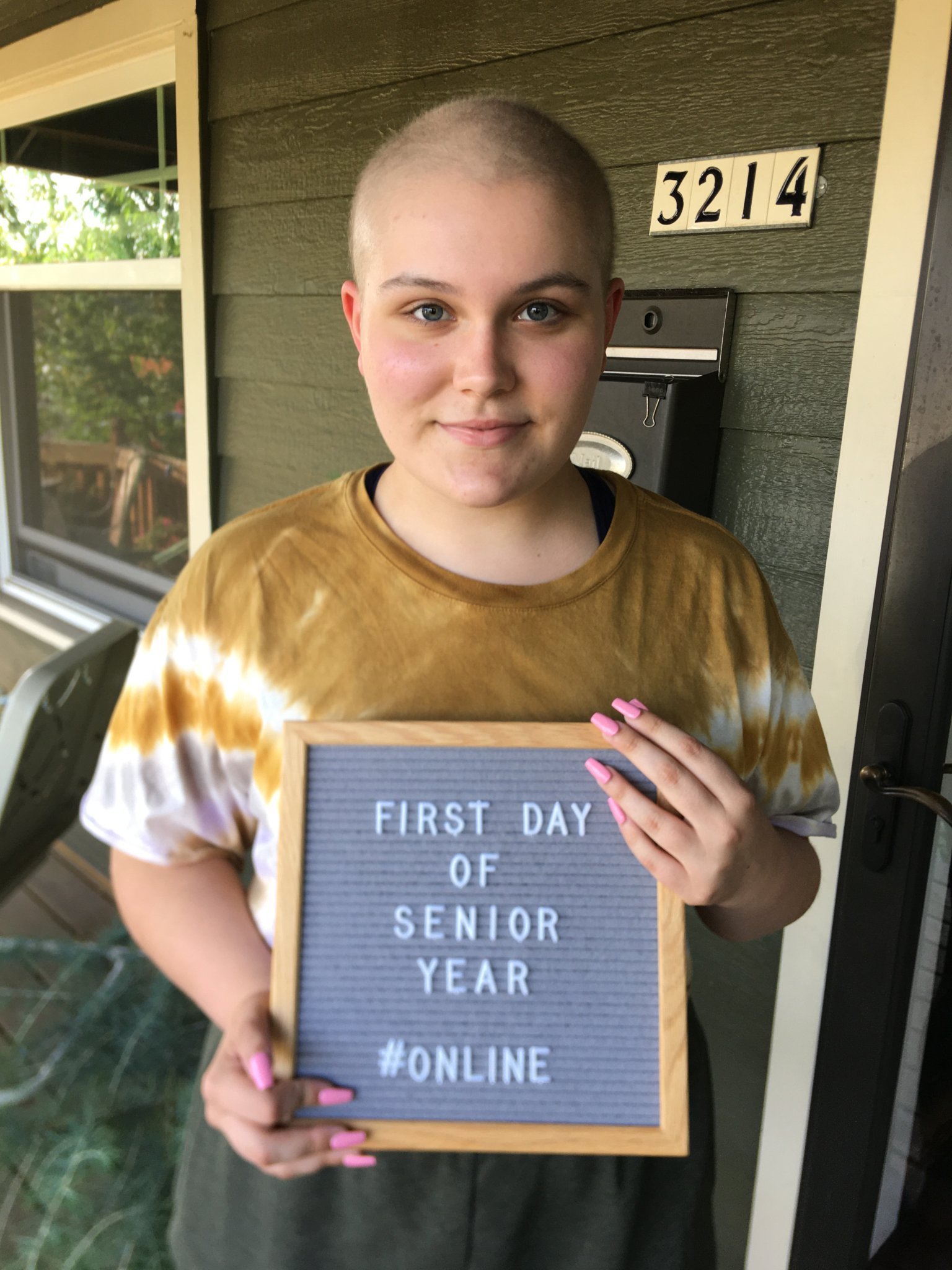
After five inpatient hospital stays with chemotherapy and rituximab infusions, nine spinal taps, and at least four CT scans, Maddie got to ring that bell, and she officially entered remission on September 10, 2020. The first year after that was rough, I'm not going to lie, with my 17-year-old figuring out how to live after such a traumatic experience. Her senior year was fully online, which was lucky since her immune system was not up to par, and we wanted to avoid COVID if we could. Remote school, as the world learned during the pandemic, isn't ideal, but it sure was lucky she had that alternative the year after chemo.
She graduated from high school in June 2021, got her first job in August, will have her associate's degree this spring, and is doing amazingly well. The future is wide open for Maddie, and I can't wait to see what it brings.