Immunotherapy uses the power of the immune system to treat blood cancer. Today it is a standard treatment that has a profound effect in some blood cancer patients, but it still falls short in others.
The Leukemia & Lymphoma Society (LLS) has been a champion of this type of cancer treatment for decades, supporting some of the earliest and most game-changing immune-based treatments for blood cancer. The advances have been astonishing, but there is so much further to go.
LLS is united with world renowned scientists, with $93 million committed to more than 70 research projects looking at ways to make immunotherapies more effective with longer lasting results. We’re also focused on supporting researchers who are working to make it safer, easier and quicker to use, and available to more patients.
So, what exactly is immunotherapy and what should patients and their families know about it?
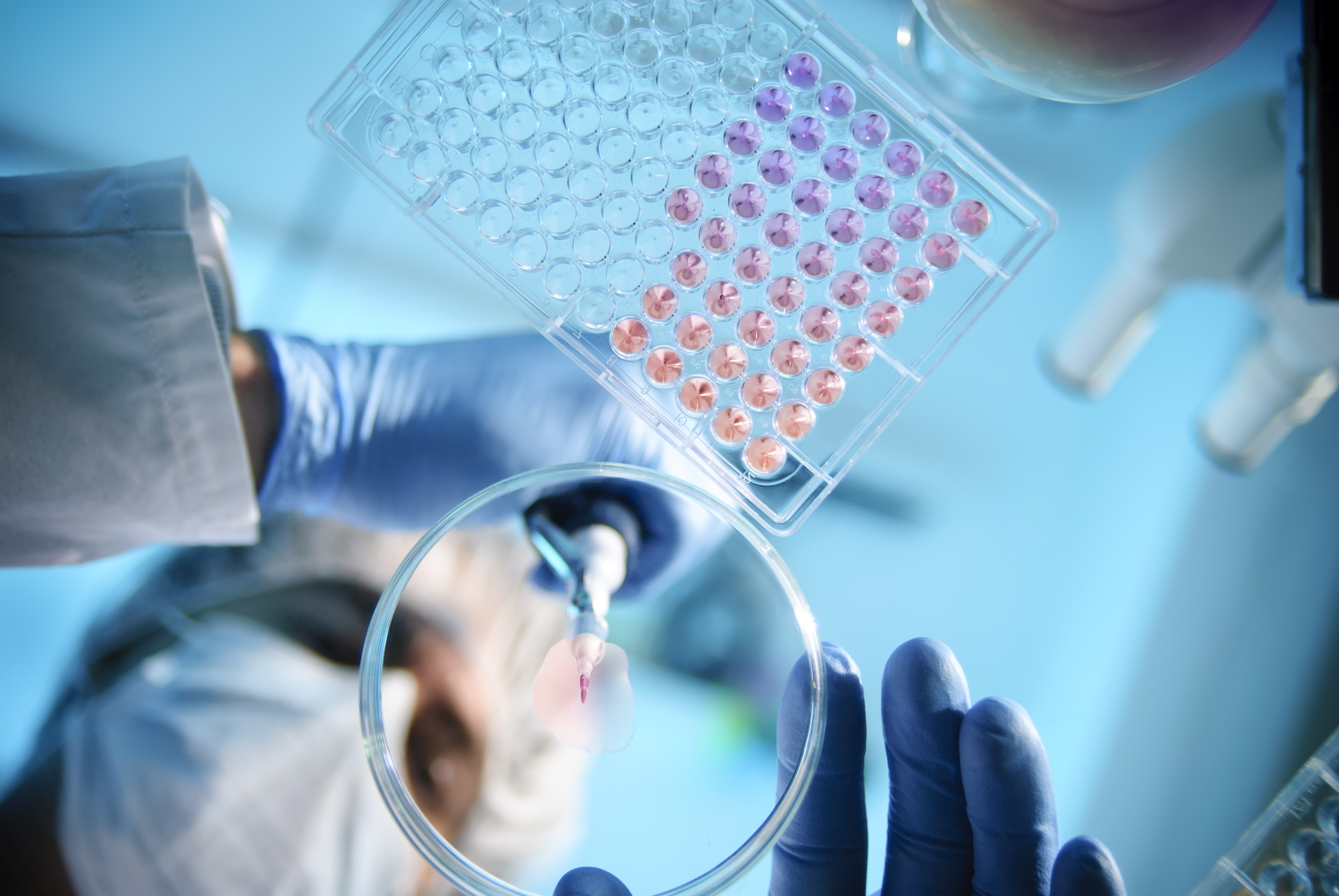
Immunotherapy stimulates, boosts, or trains the immune system to specifically target cancer
Our immune systems are incredibly complex. They can be used in many ways to treat blood cancers. These are just a few examples of how different immunotherapies work:
- Stem cell transplants can cure people with certain forms of leukemia, lymphoma, multiple myeloma, and myelodysplastic syndromes. Successful stem cell transplants generate an entirely new immune system for patients. Transplants obtained from donors, called allogeneic transplants, can kill the patient’s tumor cells as well as restart the immune system.
- Monoclonal antibodies, discovered in 1975, are lab-made versions of the antibodies our bodies make. In the case of cancer, these antibodies are trained to bind to tumor cells and recruit the patient’s immune system to kill them. Rituximab, the first cancer-fighting monoclonal antibody, approved by the FDA in 1997, is a mainline therapy for non-Hodgkin lymphoma to this day.
- Antibody drug conjugates, or ADCs, have been called biological missiles. ADCs for blood cancer combine a drug that can find specific cancer cells and release a powerful cytotoxic drug at the tumor.
- CAR T-immunotherapy works by modifying a patient’s own T cells to find and attack their blood cancer. A chimeric antigen receptor (the “CAR” in CAR-T) is added to the T cells and is trained to find a specific target usually found on certain cancer cells. In the case of lymphomas, that target is a protein called CD19. For multiple myeloma, the target is a protein called BCMA. The first CAR T cell therapy was FDA approved in 2017.
- Bispecific antibodies are a similar concept to CAR T therapy, except in this case the same antibody binds to, and brings, both the T-cell and the tumor together. The T-cell then kills the tumor cell.
- Checkpoint inhibitors block “checkpoint” proteins. These proteins exist to keep the immune system from killing off healthy cells. But cancer can be tricky—it sends signals that turn on checkpoint inhibitors, so the immune system leaves the cancer alone. Checkpoint inhibitors stop that process, taking the brakes off so the immune system can get back to doing its job.
Immunotherapy treatment options are expanding quickly
Immunotherapy has become so common that it’s easy to forget it’s also fairly new—emerging as a standard treatment for many blood cancers only over the last decade or so.
Within the last seven years, there have been 16 CAR-T FDA approvals of six different CAR-T products. They treat chronic lymphocytic leukemia, B-cell acute lymphoblastic leukemia, multiple myeloma, and many forms of non-Hodgkin lymphoma, including follicular, mantle cell and large B-cell. In the past few years, CAR T therapy has also been shown to control progression of non-blood cancers and autoimmune diseases in patients. FDA approvals for CAR T for these uses are likely soon.
Originally approved as a treatment of last resort, CAR T-cell immunotherapy has proven highly effective (at least for some patients—more on that later) and oncologists have learned how to manage their common side effects. These developments have led the U.S. Food and Drug Administration (FDA) to approve some CAR-Ts for earlier use for several types of blood cancer.
This is important for several reasons. CAR T-cell therapy is usually a “one and done” treatment that can lead to long-term remissions and even cures for some patients. Using it earlier in treatment also carries another important benefit. Later treatment may not work because by then a patient’s T cells might be too damaged from earlier treatments.
Immunotherapy generally causes fewer side effects than chemo, but it is not risk-free
The complexity of the immune system means it holds great promise in treating cancer, but it also means researchers need to look very carefully at exactly how our treatments are interacting with it.
For example, immunotherapy can cause an over-activation of the immune system, leading to fever, nausea, rapid heartbeat, low blood pressure and more. Neuropsychiatric symptoms, such as cognitive impairments and changes in mood, including anxiety and depression, may also occur.
While these conditions are usually mild, resolving on their own in most patients, they can be debilitating or even life-threatening in others. Today we know a lot more about how to treat these problems sooner to reduce their effects for most patients.
Some immunotherapies, like chemotherapies and radiation treatment, can also lead to secondary cancers. This has been a long-time paradox for doctors who treat cancer—the knowledge that treatment that can give people months or years of additional life can also leave them susceptible to other types of cancer in the future. Based on the data available so far, the benefits of CAR T-cell therapy far outweigh the risk.
Maximizing immunotherapy safety and tolerability (reducing the risk of side effects like diarrhea, fatigue and nausea) is an ongoing focus of hundreds of scientists across the world, thanks to large and ongoing investments in their work by LLS and others.
Researchers are working to improve immunotherapies
Immunotherapy doesn’t work for everyone. For example, age and co-existing conditions can change the effectiveness of checkpoint inhibitors. Another example: many forms of blood cancer and their treatments directly attack the very T-cells immunotherapies need to work. This means people who have had cancer for a while or who have received earlier treatments can have “T-cell exhaustion,” where they don’t have enough functioning T-cells to mount a response to immunotherapy treatment.
One solution being explored by LLS-funded researcher is using donor T-cells. This provides healthy T-cells, and the treatment can be ready to be taken “off the shelf” when a patient needs it instead of having to wait the weeks or more it takes to collect, modify, grow and reinfuse a patient’s own T-cells. This strategy is being evaluated in blood cancer patients by Caribou Biosciences, a company supported by LLS.
But the flip side is that the patient’s immune system may see the donor T-cells as foreign (and vice versa) setting up a war inside the patient’s body. Genetic engineering, including the exciting CRISPR technology, is poised to play a large part in the future of immunotherapy. This precision editing tool is being tested to modify certain parts of the donor T-cells, so the patient’s own T-cells won’t attack them.
This is just one of many exciting new research avenues to extend the value of CAR T-cell immunotherapy.
Conclusion
Thirty years ago, immunotherapy to treat blood cancer was just emerging and sounded like science fiction to most lay people (and a whole lot of scientists, too). Today, immunotherapies are making an enormous difference in the lives of patients and their families. But there is so much more we can accomplish. LLS has its eyes toward a future where more effective and safer immune-based treatments are available to patients at all stages or all forms of blood cancer.
If you or a loved one need personalized disease, treatment or support information, contact our Information Specialists