Search Results
Children and End of Life
Children facing end-of-life have specific needs and concerns to consider. It's important to approach them in a spirit of honesty. However, honesty doesn't mean overwhelming them with information and details that can be frightening. Honesty means honesty of feeling. Information needs to be screened and made appropriate for their needs.
Treatment
On average, individuals with essential thrombocythemia (ET) have a normal life expectancy if they are properly monitored and treated. It's important that your doctor is experienced in treating myeloproliferative neoplasms (MPNs) or works in consultation with a hematologist oncologist who has experience treating MPN patients.
Jarvis
In the fall of 2019, life was very active for me and my 4-year-old son Jarvis. I was busy working 2-3 jobs, and Jarvis was busy just being a kid. Almost every day after school we would go to the park so he could run around and play. He was even starting to get interested in bikes and wanting to learn to ride when he started to mention his feet were hurting.
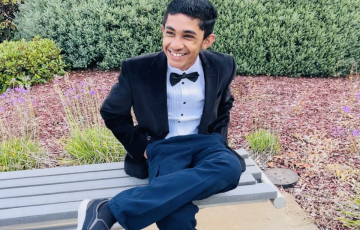
Brent
My nephew Brent Terence was a perfectly healthy 17-year-old young man, active in school, up-to-date on his routine check-ups, and had normal labs. But until the end of July 2022, Terence showed signs of extreme fatigue, confusion, loss of memory, hallucination, and an inability to keep his eyes open and walk straight. So his parents, Brenda and Tristan, decided to take him to the ER. Multiple blood tests and X-rays were done, but they couldn’t figure it out.

Jonathan
I was diagnosed with B-cell acute lymphoblastic leukemia (ALL) on July 26, 2019, and even without the involvement of a pandemic, I imagine that’s reason enough to believe that to me 2018 seems like a lifetime ago. Still, I can remember it well enough: A wide-eyed younger version of me arrived at college orientation, somehow simultaneously thrilled to begin a new chapter of his life and paralyzingly terrified of the imminent unknown.

Jennifer
On New Year's Day 2012, I was diagnosed with acute myeloid leukemia (AML). I watched the ball drop in the ICU with a nurse assigned to me. They heard my mom being asked if I needed to be resuscitated, so they proceeded with that and then to hear her respond to do everything you can for her. The seriousness of that is very overwhelming.

Austin
Four were spoken that day. Four crushing, breathtaking words, “Your son has cancer.” My world, my life, and my dreams for my son’s future suddenly halted while the rest of the world kept going on around us on May 14, 2011. Only days before, I was deciding what theme to have for his third birthday party and what outfit he would wear for his pictures. Days later, my husband and I were signing consents for the specific protocol of poison that would be pumped into Austin and having to digest the laundry list of possible side effects.
Aryan
Hello, my name is Aryan. I am 13 years old. I was almost five years old when I first got diagnosed with cancer. It started as a normal summer like always, and we were planning to go somewhere. My dad was always traveling because of work, so it was just me and my mom. I would mostly spend time at my grandparents’ house because I could play games with them. One day my dad saw a bump on the back of my head, and our pediatrician told us that it was a lymph node. My pediatric doctor told my parents that it's normal, part of recovery from a fever or cough and to monitor it.

Paul & Lynn
In 2017, after 44 years of working in the railroad industry, Paul Sauter was just starting to enjoy his retirement, when his health started to decline out of nowhere. Typically, he was in extremely good shape and enjoyed long hikes with his wife, Lynn. One day, while on a mountain climb trip in Arizona, Lynn was concerned when she noticed Paul was not his usual athletic self. When he was unable to get out of bed because of severe back pain, she knew something wasn’t right.

Santino
I know the pain of being told that you have cancer twice, but I also know the joy of being told that you have beaten cancer twice. I write this message to bring encouragement and to instill a fight in people who have had a relapse of cancer. Being told once that you have this disease is already heartbreaking, but to be told that it came back and you will need chemo again is soul-crushing.

Jamiee
During COVID, I completed my graduate degree. This was in 2020, and things started to look up. Not only did I become the first member of my family to achieve a graduate degree, I also did it pregnant. I welcomed my second child in 2020, two months after graduation. In 2021, once the world settled a bit, I began to go on a healing journey where I started working on my mental and physical health. It was amazing, I finally began feeling great about myself, had the stamina to enjoy my children, and was in a career I loved.

Russ
Shockingly I was diagnosed with acute myeloid leukemia (AML) on February 28, 2024! My wife Nancy and I were devastated and had zero background or experience with leukemia. We were sent to UCLA for treatment. What a godsend!
Be Your Child’s Advocate
Parents may need to educate other family members, friends, school personnel and healthcare providers about long-term and late effects. Here are some steps parents can take:
Chemotherapy and Drug Therapy
The main treatment for active myeloma is systemic drug therapy (meaning the drugs travel through the bloodstream to kill malignant cells). The initial therapy, or “induction therapy,” for myeloma usually includes a combination of targeted agents and/or standard chemotherapy. This therapy is often followed by stem cell transplantation in eligible patients.
Common drugs combinations for people with newly diagnosed myeloma include:
Treatment Outcomes
With the current advances in treatment and supportive care, survival rates for myeloma patients have improved significantly in the last decades. It is not unusual for myeloma patients to live for 10 years or longer after diagnosis. Outcomes are influenced by a series of patient-specific factors, including disease stage, chromosome abnormalities, age and presence of other medical problems. Patients should discuss their own potential outcomes with their doctors.
Click here to access myeloma survival statistics.

Israel
I am 39 years old, a father of two boys and one girl ― Abdias, 12 years old; Ester, 10 years old; and Ben, 9 years old ― and a husband to my wife Erin for almost 14 years.
On August 14, 2021, I suffered a serious knee injury playing basketball which inadvertently led to revealing I had a blood cancer called chronic myeloid leukemia (CML). Suddenly, instead of prepping for knee surgery, I was sent to the hospital and received an official diagnosis on September 9 after a bone marrow biopsy and what felt like a million tests.

Crystal
My story starts in early December 2024. I had been getting sick a lot that year, and it finally struck me as odd when it just wouldn’t go away. I had this intense pressure in my chest as if something was sitting on top of it. Something felt wrong. I finally realized I had to go in and get checked out; I could no longer ignore my body. Early one morning, I went to urgent care, figuring I might have pneumonia or a chest infection and that I’d be sent home with some medication.

Teresa
It took two months for the doctors to take my illness seriously. I was suffering from hip and leg pain, but the doctors thought it was caused by the sports I was playing in high school. They would send me home with pain medication.

Lyndi
In March 2019 I began feeling off...I didn't know what it was. I thought perhaps it was a loss of relationship that broke me to my core, or that fact that an old friend had asked me to be kidney donor for someone I had never know. I agreed to be tested to see if I was a possible match. Fast forward to October when I was tested a possible blood clot that had formed from all of this. I was having continual pain in my right shoulder blade.

Ariana
In the blink of an eye, our lives can crumble underneath us like a tsunami drowning the life out of a city. Many of us unknowingly stand on the edge of an eroding cliff and one slip away from relinquishing our most desired aspirations. At 19 years old, I stood inches away from the edge of that cliff when I was diagnosed with essential thrombocythemia (ET). This was one of the most defining moments in my life that propelled me into a tenacious desire to become a physician capable of fully understanding the fragility of life.
Talking About Cancer
Telling people about your diagnosis is a very personal decision. Some people with cancer choose to tell only close family. Others find it helps to let more people know about their diagnosis. Take some time to consider what and how much you would like to share about your diagnosis and how you want to share this information. By letting friends and family know about your diagnosis, you give them the chance to offer their support.
Here are some tips and things to keep in mind when telling someone about your diagnosis:
Diagnosis
An accurate diagnosis of the type of leukemia is important. The exact diagnosis helps the doctor to
- Estimate how the disease will progress
- Determine the appropriate treatment
After your doctor or clinician takes your blood, he or she sends it to a lab for a complete blood count (CBC), which shows the number of red cells, white cells and platelets in your blood.